Branch Retinal Vein Occlusion
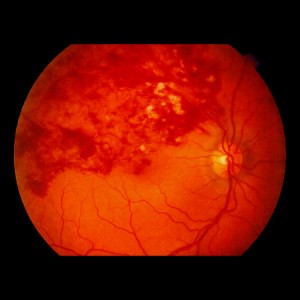 The retina is a thin sheet of nerve tissue in the back of the eye where light rays are focused and transmitted to the brain. Tiny blood vessels supply the retina with oxygen and other nutrients. Arteries deliver the blood, and the retinal veins carry it out. A retinal vein occlusion (RVO) occurs when an artery supplying blood to the eye hardens or swells and presses on a nearby vein and blocks it, making it difficult for blood to leave the eye. The blocked circulation can lead to swelling, bleeding, growth of abnormal blood vessels, and partial or total vision loss.
The retina is a thin sheet of nerve tissue in the back of the eye where light rays are focused and transmitted to the brain. Tiny blood vessels supply the retina with oxygen and other nutrients. Arteries deliver the blood, and the retinal veins carry it out. A retinal vein occlusion (RVO) occurs when an artery supplying blood to the eye hardens or swells and presses on a nearby vein and blocks it, making it difficult for blood to leave the eye. The blocked circulation can lead to swelling, bleeding, growth of abnormal blood vessels, and partial or total vision loss.
Risk Factors For Branch Retinal Vein Occlusion
BRVO is linked with aging and is commonly diagnosed in patients who are 50 years or older. Patients with high blood pressure, diabetes, and/or glaucoma are more likely to be affected by BRVO.
Some additional factors that may increase your chances of developing BRVO are:
- High-fat diet
- Lack of exercise
- Obesity
- Smoking
- High cholesterol
- Smoking
- Blood clotting (rarely)
- Inflammatory conditions (rarely)
Treatment of Branch Retinal Vein Occlusion
There is no cure, so emphasis is placed on risk management, treatment of symptoms and prevention of further vision loss. It is critical to control high blood pressure, high cholesterol, diabetes and other health conditions that increase the risk of vascular hardening, narrowing and blood clotting.
Macular swelling may be treated with intravitreal injections of medication (anti-VEGF or steroid) and/or laser photocoagulation. Neovascularization typically appears six months to a year after the occlusion. It can cause bleeding, glaucoma, retinal detachment and reduced vision in its advanced stages, so laser photocoagulation treatment is recommended to slow or stop vessel growth. If bleeding continues, a vitrectomy may be performed to remove the blood and vitreous gel. Vitrectomy can also relieve tension from a retinal detachment.


